THE CASE
A 72-year-old woman came to our internal medicine department clinic for a follow-up appointment for her fibromyalgia. Thirteen months earlier, she had sought care at our facility not only for fibromyalgia, but for insomnia, anxiety, depression, and urinary incontinence. At the time, we prescribed amitriptyline 10 mg/d—for her pain and depression—as well as clonazepam 10 mg/d and paracetamol 650 mg, as needed.
When she came in for the follow-up, she indicated that for the past 8 months, she’d been experiencing urinary retention that required her to self-catheterize 2 to 3 times a day. She said she hadn’t used other medicines or herbal products during this time.
The patient had visited her family physician several times over the previous few months, and had been referred to a urologist. During an episode of acute urinary retention, she went to the emergency department (ED), where the ED physician performed urinary catheterization and referred her to the hospital’s Urology Department. After 48 hours, she was evaluated by a urologist, who diagnosed chronic urinary retention related to a hypercontractile bladder, without any particular cause. She was advised to continue to catheterize herself when needed. She was also prescribed pyridostigmine bromide, but she stopped taking it because of abdominal pain and bloating.
Two months prior to her visit with us, the patient suffered a second acute urinary retention episode and returned to the ED. Urinary catheterization was performed for 72 hours. At her next visit to her urologist, she was told to continue self-catheterization and was prescribed silodosin 8 mg/d.
THE DIAGNOSIS
Based on the patient’s history, we suspected the urinary retention was secondary to the anticholinergic effects of amitriptyline. We were able to determine that the patient’s urinary retention was likely the result of an adverse drug reaction (ADR) by using the causality algorithm of the Spanish Pharmacovigilance System, which suggests the following criteria:1 a) a positive time sequence (ie, onset of symptoms closely followed administration of the medication), b) the existence of an ADR that is well known and consistent with the mechanism of action of the drug,2 c) symptoms that resolve after suspending the drug; d) no repeat exposure (to the adverse effects of amitriptyline) due to ethical reasons; and e) the absence of an alternative explanation for the symptoms.3
DISCUSSION
Although indicated for depression, amitriptyline is also used for other conditions, including nocturnal enuresis and chronic neuropathic pain.4 Amitriptyline exhibits anticholinergic effects that can cause symptoms related to the nervous system (agitation, disorientation, sleepiness, delirium, cognitive impairment), ocular system (blurred vision, dry eye, accommodation disturbances, increased intraocular pressure), cardiovascular system (tachycardia), gastrointestinal tract (dry mouth, paralytic ileus, constipation), urinary system (urinary retention); and skin and mucosal membranes (dryness).5,6 Anticholinergic effects can also induce hyperthermia or increase the risk of falls.5,6
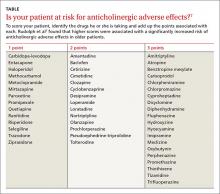
Anticholinergic medications can cause ADRs in high-risk older patients and thus are usually considered inappropriate for this patient population.6 The Anticholinergic Risk Scale (ARS) can be used to categorize medications based on their potential for anticholinergic adverse effects (TABLE).7 Amitriptyline is included in the group with the highest risk of ADRs. Amitriptyline is also included in the list of drugs that should be avoided in older adults, according to the 2012 American Geriatrics Society Beers Criteria.8
Our patient. We instructed her to stop taking amitriptyline, and her urinary retention disappeared within 48 hours. Two months later, she remained asymptomatic.
THE TAKEAWAY
Although many medications are known to cause adverse events, they can be missed when clinicians fail to pinpoint exactly when a new sign, symptom, or health problem appeared. This often leads to a chain reaction of unnecessary explorations, harmful treatment, patient suffering, and unjustified costs.9-11 Our patient had seen 4 different health care providers (a family physician, urologist, and 2 ED physicians) before we saw her and ultimately made the diagnosis. Family physicians can prevent anticholinergic ADRs by using a scale, such as the ARS, before prescribing a medication.