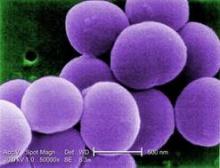
BOSTON – It’s no surprise that antibiotic resistance continues to grow, but now some Staphylococcus aureus are showing off a new trick – resistance to chlorhexidine, the antiseptic relied upon to prevent staph infections.
In a review of isolates from pediatric cancer patients, an increasing number of S. aureus became resistant to the antiseptic, Dr. J. Chase McNeil said at the annual meeting of the Pediatric Academic Societies. The jump from susceptible to resistant occurred around 2006 – 2 years after the Texas Children’s Hospital began using chlorhexidine in the weekly central line dressing changes for its cancer patients, and a year after the facility introduced chlorhexidine mouthwash up to four times each day for patients with acute myeloid leukemia.
"It’s very interesting to see this upward trend [in resistance]," he said in an interview. "Before 2007, we had none, and since then we’ve seen an increase every year."
While the clinical significance of this phenomenon remains unclear, it’s very clear that the bacteria are changing, he added.
Dr. Chase reported a review of a prospectively acquired data set, which includes all children treated at the university’s pediatric oncology facility. He and his coinvestigators looked for infections caused by S. aureus and their related complications. They also assessed the emergence of staph isolates showing the qacA/B gene, which confers a higher minimum inhibitory concentration and minimum bactericidal concentration to chlorhexidine and other quaternary ammonium compound (QAC) antiseptics. The study also examined rates of methicillin resistance.
From 2001 through 2011, 213 S. aureus infections developed in 179 patients. Infections were most commonly associated with acute lymphoblastic leukemia (43%). Other cancers were primary central nervous system malignancies (11%), acute myeloid leukemia (AML), and hematopoietic stem cell transplant (HSCT) patients (16%). Among the infections were bacteremias (40%), skin and soft tissue infections (36%) and surgical site infections (15%).
Most of the infections were methicillin-susceptible S. aureus (147); the remaining infections were methicillin resistant. Most of the methicillin-resistant S. aureus isolates were also the USA300 strain, a particularly resistant strain associated with serious, rapidly progressing infections. The USA300 isolates were responsible for 59% of the skin/soft tissue infections and 25% of the bacteremias.
Overall, 8% of the isolates were also qacA/B positive. These were more likely to be resistant to ciprofloxacin than the qacA/B-negative isolates (50% vs. 15%).
Chlorhexidine-cleansed dressing changes and catheter cleansings began in 2004 in response to a sharp increase in staph infections in AML and HSCT patients, Dr. McNeil said. These infections did drop precipitously in the following years. In 2005, AML patients began using a chlorhexidine mouthwash up to four times each day.
However, in 2006, just as the staph infection rate was improving, qacA/B resistance suddenly appeared. By 2009, 10% of infections were positive for qacA/B, and by 2011, this had risen to about 22%.
"We can’t say if the change in the microbiology of these is caused by anything, or causing anything significant, but there is definitely a temporal association," he said.
Chlorhexidine continues to be relied upon in the oncology ward, he said. By 2011, daily chlorhexidine baths became part of the standard care for neutropenic AML patients.
Among the entire group of patients with infections, 19% (37) developed a total of 58 complications. Bacteremias were associated with most of the complications (70%). A multivariate analysis showed a significant association between complicated bacteremias and AMC patients with a low lymphocyte count.
Thirteen patients with bacteremia also developed pulmonary nodules. All of these were associated with methicillin-susceptible S. aureus isolates. The nodules developed rapidly, appearing a median of 5 days after bacteremia onset. Six patients were biopsied, with S. aureus cultured from five. One nodule was a metastatic tumor. One other patient with nodules died before culture. This patient had an invasive pulmonary fungal infection.
Dr. McNeil said several factors were significantly associated with staph infections and pulmonary nodules, including HSCT, a low lymphocyte count, and low platelets.
"This isn’t surprising because it’s well known that children with malignancies are at a high risk for staph disease because of their immune compromise and a high exposure to empiric antibiotics and antiseptics."
Dr. McNeil said he had no financial declarations.